Antibiotic resistance
Antibiotic resistance is a type of drug resistance where a microorganism is able to survive exposure to an antibiotic. Genes can be transferred between bacteria in a horizontal fashion by conjugation, transduction, or transformation. Thus a gene for antibiotic resistance which had evolved via natural selection may be shared. Evolutionary stress such as exposure to antibiotics then selects for the antibiotic resistant trait. Many antibiotic resistance genes reside on plasmids, facilitating their transfer. If a bacterium carries several resistance genes, it is called multiresistant or, informally, a superbug or super bacteria.
The primary cause of antibiotic resistance is antibiotic use both within medicine and veterinary medicine. The greater the duration of exposure the greater the risk of the development of resistance irrespective of the severity of the need for antibiotics.
Contents |
Causes
The widespread use of antibiotics both inside and outside of medicine is playing a significant role in the emergence of resistant bacteria.[1] Antibiotics are often used in rearing animals for food and this use among others leads to the creation of resistant strains of bacteria. In some countries antibiotics are sold over the counter without a prescription which also leads to the creation of resistant strains. In supposedly well-regulated human medicine the major problem of the emergence of resistant bacteria is due to misuse and overuse of antibiotics by doctors as well as patients.[2] Other practices contributing towards resistance include the addition of antibiotics to the feed of livestock.[3][4] Household use of antibacterials in soaps and other products, although not clearly contributing to resistance, is also discouraged (as not being effective at infection control).[5] Also unsound practices in the pharmaceutical manufacturing industry can contribute towards the likelihood of creating antibiotic resistant strains.[6]
Certain antibiotic classes are highly associated with colonisation with superbugs compared to other antibiotic classes. The risk for colonisation increases if there is a lack of sensitivity (resistance) of the superbugs to the antibiotic used and high tissue penetration as well as broad spectrum activity against "good bacteria". In the case of MRSA, increased rates of MRSA infections are seen with glycopeptides, cephalosporins and especially quinolones.[7][8] In the case of colonisation with C difficile the high risk antibiotics include cephalosporins and in particular quinolones and clindamycin.[9][10]
In medicine
The volume of antibiotic prescribed is the major factor in increasing rates of bacterial resistance rather than compliance with antibiotics.[11] A single dose of antibiotics leads to a greater risk of resistant organisms to that antibiotic in the person for up to a year.[12]
Inappropriate prescribing of antibiotics has been attributed to a number of causes including: people who insist on antibiotics, physicians simply prescribe them as they feel they do not have time to explain why they are not necessary, physicians who do not know when to prescribe antibiotics or else are overly cautious for medical legal reasons.[13] A third of people for example believe that antibiotics are effective for the common cold[14] and 22% of people do not finish a course of antibiotics primarily due to that fact that they feel better (varying from 10% to 44% depending on the country).[15] Compliance with once daily antibiotics is better than with twice daily antibiotics.[16] Sub optimum antibiotic concentrations in critically ill people increase the frequency of antibiotic resistance organisms.[17] While taking antibiotics doses less than those recommended may increase rates of resistance, shortening the course of antibiotics may actually decrease rates of resistance.[11][18]
Poor hand hygiene by hospital staff has been associated with the spread of resistant organisms[19] and an increase in hand washing compliance results in decreased rates of these organisms.[20]
Role of other animals
Drugs are used in animals that are used as human food, such as cows, pigs, chickens, fish, etc., and these drugs can affect the safety of the meat, milk, and eggs produced from those animals and can be the source of superbugs. For example, farm animals, particularly pigs, are believed to be able to infect people with MRSA.[21] The resistant bacteria in animals due to antibiotic exposure can be transmitted to humans via three pathways, those being through the consumption of meat, from close or direct contact with animals, or through the environment.[22]
The World Health Organization concluded that antibiotics as growth promoters in animal feeds should be prohibited (in the absence of risk assessments). In 1998, European Union health ministers voted to ban four antibiotics widely used to promote animal growth (despite their scientific panel's recommendations). Regulation banning the use of antibiotics in European feed, with the exception of two antibiotics in poultry feeds, became effective in 2006.[23] In Scandinavia, there is evidence that the ban has led to a lower prevalence of antimicrobial resistance in (non-hazardous) animal bacterial populations.[24] In the USA federal agencies do not collect data on antibiotic use in animals but animal to human spread of drug resistant organisms has been demonstrated in research studies. Antibiotics are still used in U.S. animal feed—along with other ingredients which have safety concerns.[4][25]
Growing U.S. consumer concern about using antibiotics in animal feed has led to a niche market of "antibiotic-free" animal products, but this small market is unlikely to change entrenched industry-wide practices.[26]
In 2001, the Union of Concerned Scientists estimated that greater than 70% of the antibiotics used in the US are given to food animals (e.g. chickens, pigs and cattle) in the absence of disease.[27] In 2000 the US Food and Drug Administration (FDA) announced their intention to revoke approval of fluoroquinolone use in poultry production because of substantial evidence linking it to the emergence of fluoroquinolone resistant campylobacter infections in humans. The final decision to ban fluoroquinolones from use in poultry production was not made until five years later because of challenges from the food animal and pharmaceutical industries.[28] Today, there are two federal bills (S. 549[29] and H.R. 962[30]) aimed at phasing out "non-therapeutic" antibiotics in US food animal production.
Mechanisms
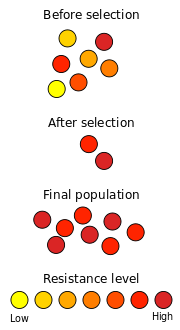
Antibiotic resistance can be a result of horizontal gene transfer,[31] and also of unlinked point mutations in the pathogen genome and a rate of about 1 in 108 per chromosomal replication. The antibiotic action against the pathogen can be seen as an environmental pressure; those bacteria which have a mutation allowing them to survive will live on to reproduce. They will then pass this trait to their offspring, which will result in a fully resistant colony.
The four main mechanisms by which microorganisms exhibit resistance to antimicrobials are:
- Drug inactivation or modification: e.g. enzymatic deactivation of Penicillin G in some penicillin-resistant bacteria through the production of β-lactamases.
- Alteration of target site: e.g. alteration of PBP—the binding target site of penicillins—in MRSA and other penicillin-resistant bacteria.
- Alteration of metabolic pathway: e.g. some sulfonamide-resistant bacteria do not require para-aminobenzoic acid (PABA), an important precursor for the synthesis of folic acid and nucleic acids in bacteria inhibited by sulfonamides. Instead, like mammalian cells, they turn to utilizing preformed folic acid.
- Reduced drug accumulation: by decreasing drug permeability and/or increasing active efflux (pumping out) of the drugs across the cell surface.[32]
There are three known mechanisms of fluoroquinolone resistance. Some types of efflux pumps can act to decrease intracellular quinolone concentration. In gram-negative bacteria, plasmid-mediated resistance genes produce proteins that can bind to DNA gyrase, protecting it from the action of quinolones. Finally, mutations at key sites in DNA gyrase or Topoisomerase IV can decrease their binding affinity to quinolones, decreasing the drug's effectiveness.[33] Research has shown that the bacterial protein LexA may play a key role in the acquisition of bacterial mutations giving resistance to quinolones and rifampicin.[34]
Antibiotic resistance can also be introduced artificially into a microorganism through laboratory protocols, sometimes used as a selectable marker to examine the mechanisms of gene transfer or to identify individuals that absorbed a piece of DNA that included the resistance gene and another gene of interest.
Resistant pathogens
Staphylococcus aureus
Staphylococcus aureus (colloquially known as "Staph aureus" or a Staph infection) is one of the major resistant pathogens. Found on the mucous membranes and the human skin of around a third of the population, it is extremely adaptable to antibiotic pressure. It was one of the earlier bacteria in which penicillin resistance was found—in 1944, just four years after the drug started being mass-produced. Methicillin was then the antibiotic of choice, but has since been replaced by oxacillin due to significant kidney toxicity. MRSA (methicillin-resistant Staphylococcus aureus) was first detected in Britain in 1961 and is now "quite common" in hospitals. MRSA was responsible for 37% of fatal cases of sepsis in the UK in 1999, up from 4% in 1991. Half of all S. aureus infections in the US are resistant to penicillin, methicillin, tetracycline and erythromycin.
This left vancomycin as the only effective agent available at the time. However, strains with intermediate (4-8 ug/ml) levels of resistance, termed GISA (glycopeptide intermediate Staphylococcus aureus) or VISA (vancomycin intermediate Staphylococcus aureus), began appearing in the late 1990s. The first identified case was in Japan in 1996, and strains have since been found in hospitals in England, France and the US. The first documented strain with complete (>16 ug/ml) resistance to vancomycin, termed VRSA (Vancomycin-resistant Staphylococcus aureus) appeared in the United States in 2002.
A new class of antibiotics, oxazolidinones, became available in the 1990s, and the first commercially available oxazolidinone, linezolid, is comparable to vancomycin in effectiveness against MRSA. Linezolid-resistance in Staphylococcus aureus was reported in 2003.
CA-MRSA (Community-acquired MRSA) has now emerged as an epidemic that is responsible for rapidly progressive, fatal diseases including necrotizing pneumonia, severe sepsis and necrotizing fasciitis.[35] Methicillin-resistant Staphylococcus aureus (MRSA) is the most frequently identified antimicrobial drug-resistant pathogen in US hospitals. The epidemiology of infections caused by MRSA is rapidly changing. In the past 10 years, infections caused by this organism have emerged in the community. The 2 MRSA clones in the United States most closely associated with community outbreaks, USA400 (MW2 strain, ST1 lineage) and USA300, often contain Panton-Valentine leukocidin (PVL) genes and, more frequently, have been associated with skin and soft tissue infections. Outbreaks of community-associated (CA)-MRSA infections have been reported in correctional facilities, among athletic teams, among military recruits, in newborn nurseries, and among men who have sex with men. CA-MRSA infections now appear to be endemic in many urban regions and cause most CA-S. aureus infections.[36]
Streptococcus and Enterococcus
Streptococcus pyogenes (Group A Streptococcus: GAS) infections can usually be treated with many different antibiotics. Early treatment may reduce the risk of death from invasive group A streptococcal disease. However, even the best medical care does not prevent death in every case. For those with very severe illness, supportive care in an intensive care unit may be needed. For persons with necrotizing fasciitis, surgery often is needed to remove damaged tissue.[37] Strains of S. pyogenes resistant to macrolide antibiotics have emerged, however all strains remain uniformly sensitive to penicillin.[38]
Resistance of Streptococcus pneumoniae to penicillin and other beta-lactams is increasing worldwide. The major mechanism of resistance involves the introduction of mutations in genes encoding penicillin-binding proteins. Selective pressure is thought to play an important role, and use of beta-lactam antibiotics has been implicated as a risk factor for infection and colonization. Streptococcus pneumoniae is responsible for pneumonia, bacteremia, otitis media, meningitis, sinusitis, peritonitis and arthritis.[38]
Penicillin-resistant pneumonia caused by Streptococcus pneumoniae (commonly known as pneumococcus), was first detected in 1967, as was penicillin-resistant gonorrhea. Resistance to penicillin substitutes is also known as beyond S. aureus. By 1993 Escherichia coli was resistant to five fluoroquinolone variants. Mycobacterium tuberculosis is commonly resistant to isoniazid and rifampin and sometimes universally resistant to the common treatments. Other pathogens showing some resistance include Salmonella, Campylobacter, and Streptococci.
Enterococcus faecium is another superbug found in hospitals. Penicillin-Resistant Enterococcus was seen in 1983, vancomycin-resistant enterococcus (VRE) in 1987, and Linezolid-Resistant Enterococcus (LRE) in the late 1990s.
Pseudomonas aeruginosa
Pseudomonas aeruginosa is a highly prevalent opportunistic pathogen. One of the most worrisome characteristics of P. aeruginosa consists in its low antibiotic susceptibility. This low susceptibility is attributable to a concerted action of multidrug efflux pumps with chromosomally-encoded antibiotic resistance genes (e.g. mexAB-oprM, mexXY etc.) and the low permeability of the bacterial cellular envelopes[39]. Besides intrinsic resistance, P. aeruginosa easily develop acquired resistance either by mutation in chromosomally-encoded genes, or by the horizontal gene transfer of antibiotic resistance determinants. Development of multidrug resistance by P. aeruginosa isolates requires several different genetic events that include acquisition of different mutations and/or horizontal transfer of antibiotic resistance genes. Hypermutation favours the selection of mutation-driven antibiotic resistance in P. aeruginosa strains producing chronic infections, whereas the clustering of several different antibiotic resistance genes in integrons favours the concerted acquisition of antibiotic resistance determinants. Some recent studies have shown that phenotypic resistance associated to biofilm formation or to the emergence of small-colony-variants may be important in the response of P. aeruginosa populations to antibiotics treatment.[40]
Clostridium difficile
Clostridium difficile is a nosocomial pathogen that causes diarrheal disease in hospitals world wide.[41][42] Clindamycin-resistant C. difficile was reported as the causative agent of large outbreaks of diarrheal disease in hospitals in New York, Arizona, Florida and Massachusetts between 1989 and 1992.[43] Geographically dispersed outbreaks of C. difficile strains resistant to fluoroquinolone antibiotics, such as Cipro (ciprofloxacin) and Levaquin (levofloxacin), were also reported in North America in 2005.[44]
Salmonella and E. coli
Escherichia coli and Salmonella come directly from contaminated food. Of the meat that is contaminated with E. coli, eighty percent of the bacteria are resistant to one or more drugs made; it causes bladder infections that are resistant to antibiotics (“HSUS Fact Sheet”). Salmonella was first found in humans in the 1970s and in some cases is resistant to as many as nine different antibiotics (“HSUS Fact Sheet”). When both bacterium are spread, serious health conditions arise. Many people are hospitalized each year after becoming infected, and some die as a result.
Acinetobacter baumannii
On November 5, 2004, the Centers for Disease Control and Prevention (CDC) reported an increasing number of Acinetobacter baumannii bloodstream infections in patients at military medical facilities in which service members injured in the Iraq/Kuwait region during Operation Iraqi Freedom and in Afghanistan during Operation Enduring Freedom were treated. Most of these showed multidrug resistance (MRAB), with a few isolates resistant to all drugs tested.[45][46]
Alternatives
Prevention
Rational use of antibiotics may reduce the chances of development of opportunistic infection by antibiotic-resistant bacteria due to dysbacteriosis. In one study the use of fluoroquinolones are clearly associated with Clostridium difficile infection, which is a leading cause of nosocomial diarrhea in the United States,[47] and a major cause of death, worldwide.[48]
There is clinical evidence that topical dermatological preparations containing tea tree oil and thyme oil may be effective in preventing transmittal of CA-MRSA.[49]
Vaccines do not suffer the problem of resistance because a vaccine enhances the body's natural defenses, while an antibiotic operates separately from the body's normal defenses. Nevertheless, new strains may evolve that escape immunity induced by vaccines; for example an update Influenza vaccine is needed each year.
While theoretically promising, anti-staphylococcal vaccines have shown limited efficacy, because of immunological variation between Staphylococcus species, and the limited duration of effectiveness of the antibodies produced. Development and testing of more effective vaccines is under way.
The Australian Commonwealth Scientific and Industrial Research Organization (CSIRO), realizing the need for the reduction of antibiotic use, has been working on two alternatives. One alternative is to prevent diseases by adding cytokines instead of antibiotics to animal feed. These proteins are made in the animal body "naturally" after a disease and are not antibiotics so they do not contribute to the antibiotic resistance problem. Furthermore, studies on using cytokines have shown that they also enhance the growth of animals like the antibiotics now used, but without the drawbacks of non-therapeutic antibiotic use. Cytokines have the potential to achieve the animal growth rates traditionally sought by the use of antibiotics without the contribution of antibiotic resistance associated with the widespread non-therapeutic uses of antibiotics currently utilized in the food animal production industries. Additionally, CSIRO is working on vaccines for diseases.
Phage therapy
Phage therapy, an approach that has been extensively researched and utilized as a therapeutic agent for over 60 years, especially in the Soviet Union, is an alternative that might help with the problem of resistance. Phage therapy was widely used in the United States until the discovery of antibiotics, in the early 1940s. Bacteriophages or "phages" are viruses that invade bacterial cells and, in the case of lytic phages, disrupt bacterial metabolism and cause the bacterium to lyse. Phage therapy is the therapeutic use of lytic bacteriophages to treat pathogenic bacterial infections.[50][51][52]
Bacteriophage therapy is an important alternative to antibiotics in the current era of multidrug resistant pathogens. A review of studies that dealt with the therapeutic use of phages from 1966–1996 and few latest ongoing phage therapy projects via internet showed: phages were used topically, orally or systemically in Polish and Soviet studies. The success rate found in these studies was 80–95% with few gastrointestinal or allergic side effects. British studies also demonstrated significant efficacy of phages against Escherichia coli, Acinetobacter spp., Pseudomonas spp and Staphylococcus aureus. US studies dealt with improving the bioavailability of phage. Phage therapy may prove as an important alternative to antibiotics for treating multidrug resistant pathogens.[53][54]
Research
New medications
Until recently, research and development (R&D) efforts have provided new drugs in time to treat bacteria that became resistant to older antibiotics. That is no longer the case. The potential crisis at hand is the result of a marked decrease in industry R&D, and the increasing prevalence of resistant bacteria. Infectious disease physicians are alarmed by the prospect that effective antibiotics may not be available to treat seriously ill patients in the near future.
The pipeline of new antibiotics is drying up. Major pharmaceutical companies are losing interest in the antibiotics market because these drugs may not be as profitable as drugs that treat chronic (long-term) conditions and lifestyle issues.[55]
The resistance problem demands that a renewed effort be made to seek antibacterial agents effective against pathogenic bacteria resistant to current antibiotics. One of the possible strategies towards this objective is the rational localization of bioactive phytochemicals. Plants have an almost limitless ability to synthesize aromatic substances, most of which are phenols or their oxygen-substituted derivatives such as tannins. Most are secondary metabolites, of which at least 12,000 have been isolated, a number estimated to be less than 10% of the total. In many cases, these substances serve as plant defense mechanisms against predation by microorganisms, insects, and herbivores. Many of the herbs and spices used by humans to season food yield useful medicinal compounds including those having antibacterial activity.[56][57][58]
Traditional healers have long used plants to prevent or cure infectious conditions. Many of these plants have been investigated scientifically for antimicrobial activity and a large number of plant products have been shown to inhibit growth of pathogenic bacteria. A number of these agents appear to have structures and modes of action that are distinct from those of the antibiotics in current use, suggesting that cross-resistance with agents already in use may be minimal. For example the combination of 5'-methoxyhydnocarpine and berberine in herbs like Hydrastis canadensis and Berberis vulgaris can block the MDR-pumps that cause multidrug resistance. This has been shown for Staphylococcus aureus.[59]
Archaeocins is the name given to a new class of potentially useful antibiotics that are derived from the Archaea group of organisms. Eight archaeocins have been partially or fully characterized, but hundreds of archaeocins are believed to exist, especially within the haloarchaea. The prevalence of archaeocins is unknown simply because no one has looked for them. The discovery of new archaeocins hinges on recovery and cultivation of archaeal organisms from the environment. For example, samples from a novel hypersaline field site, Wilson Hot Springs, recovered 350 halophilic organisms; preliminary analysis of 75 isolates showed that 48 were archaeal and 27 were bacterial.[60]
In research published on October 17, 2008 in Cell, a team of scientists pinpointed the place on bacteria where the antibiotic myxopyronin launches its attack, and why that attack is successful. The myxopyronin binds to and inhibits the crucial bacterial enzyme, RNA polymerase. The myxopyronin changes the structure of the switch-2 segment of the enzyme, inhibiting its function of reading and transmitting DNA code. This prevents RNA polymerase from delivering genetic information to the ribosomes, causing the bacteria to die.[61]
One of the major causes of antibiotic resistance is the decrease of effective drug concentrations at their target place, due to the increased action of ABC transporters. Since ABC transporter blockers can be used in combination with current drugs to increase their effective intracellular concentration, the possible impact of ABC transporter inhibitors is of great clinical interest. ABC transporter blockers that may be useful to increase the efficacy of current drugs have entered clinical trials and are available to be used in therapeutic regimes.[62]
Applications
Antibiotic resistance is an important tool for genetic engineering. By constructing a plasmid which contains an antibiotic resistance gene as well as the gene being engineered or expressed, a researcher can ensure that when bacteria replicate, only the copies which carry along the plasmid survive. This ensures that the gene being manipulated passes along when the bacteria replicates.
The most commonly used antibiotics in genetic engineering are generally "older" antibiotics which have largely fallen out of use in clinical practice. These include:
- ampicillin
- kanamycin
- tetracycline
- chloramphenicol
Industrially the use of antibiotic resistance is disfavored since maintaining bacterial cultures would require feeding them large quantities of antibiotics. Instead, the use of auxotrophic bacterial strains (and function-replacement plasmids) is preferred.
See also
- Antibiotic misuse
- Antibiotic tolerance
- Drug resistance
- Multidrug resistance
- Multidrug tolerance
- Antibacterial soap
- Bacterial conjugation
- Drug of last resort
- Efflux
- Nosocomial infection
- Pesticide resistance
- LexA
- Tuberculosis
- List of environment topics
- Broad-spectrum antibiotic
- Center for Disease Dynamics, Economics & Policy
References
- Soulsby EJ (2005). "Resistance to antimicrobials in humans and animals". BMJ 331 (7527): 1219–20. doi:10.1136/bmj.331.7527.1219. PMID 16308360. PMC 1289307. http://www.bmj.com/cgi/content/full/331/7527/1219.
- Arias, Cesar A.; Murray, BE (2009). "Antibiotic-Resistant Bugs in the 21st Century — A Clinical Super-Challenge". New England Journal of Medicine 360 (5): 439–443. doi:10.1056/NEJMp0804651. PMID 19179312.
- “Alternatives to Antibiotics Reduce Animal Disease”. Commonwealth Scientific and Industrial Research Organization. 9 Jan., 2006. 16 Apr., 2009.
Footnotes
- ↑ Goossens H, Ferech M, Vander Stichele R, Elseviers M (2005). "Outpatient antibiotic use in Europe and association with resistance: a cross-national database study". Lancet 365 (9459): 579–87. doi:10.1016/S0140-6736(05)17907-0. PMID 15708101.
- ↑ WHO (January 2002). "Use of antimicrobials outside human medicine and resultant antimicrobial resistance in humans". World Health Organization. http://www.who.int/mediacentre/factsheets/fs268/en/index.html.
- ↑ Dan Ferber (4 January 2002). "Livestock Feed Ban Preserves Drugs' Power". Science 295 (5552): 27–28. doi:10.1126/science.295.5552.27a. PMID 11778017.
- ↑ 4.0 4.1 Mathew AG, Cissell R, Liamthong S (2007). "Antibiotic resistance in bacteria associated with food animals: a United States perspective of livestock production". Foodborne Pathog. Dis. 4 (2): 115–33. doi:10.1089/fpd.2006.0066. PMID 17600481.
- ↑ "Are antibacterial-containing products (soaps, household cleaners, etc.) better for preventing the spread of infection? Does their use add to the problem of resistance?", Antibiotic Resistance Questions & Answers, Centers for Disease Control and Prevention, Atlanta, Georgia, USA, accessed November 17, 2009
- ↑ Larsson, DG.; Fick, J. (Jan 2009). "Transparency throughout the production chain -- a way to reduce pollution from the manufacturing of pharmaceuticals?". Regul Toxicol Pharmacol 53 (3): 161. doi:10.1016/j.yrtph.2009.01.008. PMID 19545507.
- ↑ Tacconelli E, De Angelis G, Cataldo MA, Pozzi E, Cauda R (January 2008). "Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis". J. Antimicrob. Chemother. 61 (1): 26–38. doi:10.1093/jac/dkm416. PMID 17986491. http://jac.oxfordjournals.org/cgi/content/full/61/1/26.
- ↑ Muto, CA.; Jernigan, JA.; Ostrowsky, BE.; Richet, HM.; Jarvis, WR.; Boyce, JM.; Farr, BM. (May 2003). "SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus.". Infect Control Hosp Epidemiol 24 (5): 362–86. doi:10.1086/502213. PMID 12785411.
- ↑ Dr Ralf-Peter Vonberg. "Clostridium difficile: a challenge for hospitals". European Center for Disease Prevention and Control. Institute for Medical Microbiology and Hospital Epidemiology: IHE. http://www.ihe-online.com/feature-articles/clostridium-difficile-a-challenge-for-hospitals/trackback/1/index.html. Retrieved 27 July 2009.
- ↑ Kuijper, EJ.; van Dissel, JT.; Wilcox, MH. (Aug 2007). "Clostridium difficile: changing epidemiology and new treatment options.". Curr Opin Infect Dis 20 (4): 376–83. doi:10.1097/QCO.0b013e32818be71d. PMID 17609596.
- ↑ 11.0 11.1 Pechère JC (September 2001). "Patients' interviews and misuse of antibiotics". Clin. Infect. Dis. 33 Suppl 3: S170–3. doi:10.1086/321844. PMID 11524715.
- ↑ "Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis -- Costelloe et al. 340: c2096 -- BMJ". http://www.bmj.com/cgi/content/full/340/may18_2/c2096.
- ↑ Arnold SR, Straus SE (2005). "Interventions to improve antibiotic prescribing practices in ambulatory care". Cochrane Database Syst Rev (4): CD003539. doi:10.1002/14651858.CD003539.pub2. PMID 16235325.
- ↑ McNulty CA, Boyle P, Nichols T, Clappison P, Davey P (August 2007). "The public's attitudes to and compliance with antibiotics". J. Antimicrob. Chemother. 60 Suppl 1: i63–8. doi:10.1093/jac/dkm161. PMID 17656386.
- ↑ Pechère JC, Hughes D, Kardas P, Cornaglia G (March 2007). "Non-compliance with antibiotic therapy for acute community infections: a global survey". Int. J. Antimicrob. Agents 29 (3): 245–53. doi:10.1016/j.ijantimicag.2006.09.026. PMID 17229552.
- ↑ Kardas P (March 2007). "Comparison of patient compliance with once-daily and twice-daily antibiotic regimens in respiratory tract infections: results of a randomized trial". J. Antimicrob. Chemother. 59 (3): 531–6. doi:10.1093/jac/dkl528. PMID 17289766.
- ↑ Thomas JK, Forrest A, Bhavnani SM, et al. (March 1998). "Pharmacodynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy". Antimicrob. Agents Chemother. 42 (3): 521–7. PMID 9517926.
- ↑ Li JZ, Winston LG, Moore DH, Bent S (September 2007). "Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis". Am. J. Med. 120 (9): 783–90. doi:10.1016/j.amjmed.2007.04.023. PMID 17765048.
- ↑ Girou E, Legrand P, Soing-Altrach S, et al. (October 2006). "Association between hand hygiene compliance and methicillin-resistant Staphylococcus aureus prevalence in a French rehabilitation hospital". Infect Control Hosp Epidemiol 27 (10): 1128–30. doi:10.1086/507967. PMID 17006822.
- ↑ Swoboda SM, Earsing K, Strauss K, Lane S, Lipsett PA (February 2004). "Electronic monitoring and voice prompts improve hand hygiene and decrease nosocomial infections in an intermediate care unit". Crit. Care Med. 32 (2): 358–63. doi:10.1097/01.CCM.0000108866.48795.0F. PMID 14758148.
- ↑ "Drug Resistant Infections: Riding Piggyback". The Economist. November 29, 2007. http://www.economist.com/displaystory.cfm?story_id=10205187&fsrc=RSS.
- ↑ Schneider K, Garrett L (June 19, 2009). "Non-therapeutic Use of Antibiotics in Animal Agriculture, Corresponding Resistance Rates, and What Can be Done About It". http://www.cgdev.org/content/article/detail/1422307/.
- ↑ Castanon J.I. (2007). "History of the use of antibiotic as growth promoters in European poultry feeds". Poult. Sci. 86 (11): 2466–71. doi:10.3382/ps.2007-00249. PMID 17954599.
- ↑ Bengtsson B., Wierup M. (2006). "Antimicrobial resistance in Scandinavia after ban of antimicrobial growth promoters". Anim. Biotechnol. 17 (2): 147–56. doi:10.1080/10495390600956920. PMID 17127526.
- ↑ Sapkota AR, Lefferts LY, McKenzie S, Walker P (May 2007). "What do we feed to food-production animals? A review of animal feed ingredients and their potential impacts on human health". Environ. Health Perspect. 115 (5): 663–70. doi:10.1289/ehp.9760. PMID 17520050.
- ↑ Baker R (2006). "Health management with reduced antibiotic use - the U.S. experience". Anim. Biotechnol. 17 (2): 195–205. doi:10.1080/10495390600962274. PMID 17127530.
- ↑ Executive summary from the UCS report "Hogging It: Estimates of Antimicrobial Abuse in Livestock", January 2001
- ↑ Nelson, JM.; Chiller, TM.; Powers, JH.; Angulo, FJ. (Apr 2007). "Fluoroquinolone-resistant Campylobacter species and the withdrawal of fluoroquinolones from use in poultry: a public health success story." (PDF). Clin Infect Dis 44 (7): 977–80. doi:10.1086/512369. PMID 17342653. http://www.journals.uchicago.edu/doi/pdf/10.1086/512369.
- ↑ US Senate Bill S. 549: Preservation of Antibiotics for Medical Treatment Act of 2007
- ↑ US House Bill H.R. 962: Preservation of Antibiotics for Medical Treatment Act of 2007
- ↑ Ochiai, K., Yamanaka, T Kimura K and Sawada, O (1959) Inheritance of drug resistance (and its transfer) between Shigella strains and Between Shigella and E.coli strains. Hihon Iji Shimpor 1861: 34 (in Japanese)
- ↑ Li, X, Nikadio H (2009). "Efflux-mediated drug resistance in bacteria: an update.". Drug 69 (12): 1555–623. doi:10.2165/11317030-000000000-00000. PMID 19678712.
- ↑ Robicsek A, Jacoby GA, Hooper DC (October 2006). "The worldwide emergence of plasmid-mediated quinolone resistance". Lancet Infect Dis 6 (10): 629–40. doi:10.1016/S1473-3099(06)70599-0. PMID 17008172. http://linkinghub.elsevier.com/retrieve/pii/S1473-3099(06)70599-0.
- ↑ Cirz RT, Chin JK, Andes DR, de Crécy-Lagard V, Craig WA, Romesberg FE (2005). "Inhibition of mutation and combating the evolution of antibiotic resistance". PLoS Biol. 3 (6): e176. doi:10.1371/journal.pbio.0030176. PMID 15869329. PMC 1088971. http://biology.plosjournals.org/perlserv/?request=get-document&doi=10.1371/journal.pbio.0030176.
- ↑ Boyle-Vavra S, Daum RS (2007). "Community-acquired methicillin-resistant Staphylococcus aureus: the role of Panton-Valentine leukocidin". Lab. Invest. 87 (1): 3–9. doi:10.1038/labinvest.3700501. PMID 17146447.
- ↑ Maree CL, Daum RS, Boyle-Vavra S, Matayoshi K, Miller LG (2007). "Community-associated methicillin-resistant Staphylococcus aureus isolates causing healthcare-associated infections". Emerging Infect. Dis. 13 (2): 236–42. doi:10.3201/eid1302.060781. PMID 17479885. PMC 2725868. http://www.cdc.gov/eid/content/13/2/236.htm?s_cid=eid236_e.
- ↑ Division of Bacterial and Mycotic Diseases (2005-10-11). "Group A Streptococcal (GAS) Disease (strep throat, necrotizing fasciitis, impetigo) -- Frequently Asked Questions". Centers for Disease Control and Prevention. http://www.cdc.gov/ncidod/dbmd/diseaseinfo/groupastreptococcal_g.htm. Retrieved 2007-12-11.
- ↑ 38.0 38.1 Albrich WC, Monnet DL, Harbarth S (2004). "Antibiotic selection pressure and resistance in Streptococcus pneumoniae and Streptococcus pyogenes". Emerging Infect. Dis. 10 (3): 514–7. PMID 15109426. http://www.cdc.gov/ncidod/eid/vol10no3/03-0252.htm.
- ↑ PMID 14706082 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ Cornelis P (editor). (2008). Pseudomonas: Genomics and Molecular Biology (1st ed.). Caister Academic Press. ISBN 978-1-904455-19-6. http://www.horizonpress.com/pseudo.
- ↑ Gerding D.N., Johnson S., Peterson L.R., Mulligan M.E. and Silva J. Jr. (1995). Clostridium difficile-associated diarrhea and colitis. Infect. Control. Hosp. Epidemiol. 16:459-477.
- ↑ McDonald L (2005). "Clostridium difficile: responding to a new threat from an old enemy" (PDF). Infect. Control. Hosp. Epidemiol. 26 (8): 672–5. doi:10.1086/502600. PMID 16156321. http://www.cdc.gov/ncidod/dhqp/pdf/infDis/Cdiff_ICHE08_05.pdf.
- ↑ Johnson S., Samore M.H., Farrow K.A (1999). "Epidemics of diarrhea caused by a clindamycin-resistant strain of Clostridium difficile in four hospitals". New England Journal of Medicine 341 (23): 1645–1651. doi:10.1056/NEJM199911253412203. PMID 16322602. http://content.nejm.org/cgi/content/full/341/22/1645.
- ↑ Loo V, Poirier L, Miller M (2005). "A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality". N Engl J Med 353 (23): 2442–9. doi:10.1056/NEJMoa051639. PMID 16322602.
- ↑ Centers for Disease Control and Prevention (CDC) (2004). "Acinetobacter baumannii infections among patients at military medical facilities treating injured U.S. service members, 2002-2004". MMWR Morb. Mortal. Wkly. Rep. 53 (45): 1063–6. PMID 15549020. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5345a1.htm.
- ↑ Medscape abstract on Acinetobacter baumannii: Acinetobacter baumannii: An Emerging Multidrug-resistant Threat.
- ↑ McCusker ME, Harris AD, Perencevich E, Roghmann MC (2003). "Fluoroquinolone use and Clostridium difficile-associated diarrhea". Emerging Infect. Dis. 9 (6): 730–3. PMID 12781017. http://www.cdc.gov/ncidod/eid/vol9no6/02-0385.htm.
- ↑ Frost F, Craun GF, Calderon RL (1998). "Increasing hospitalization and death possibly due to Clostridium difficile diarrheal disease". Emerging Infect. Dis. 4 (4): 619–25. doi:10.3201/eid0404.980412. PMID 9866738. PMC 2640242. http://www.cdc.gov/ncidod/eid/vol4no4/frost.htm.
- ↑ David T. Bearden, George P. Allen, and J. Mark Christensen, "Comparative in vitro activities of topical wound care products against community-associated methicillin-resistant Staphylococcus aureus," The Journal of Antimicrobial Chemotherapy, June 30, 2008, Vol. 62, Number 4, pp. 769–772. [1]
- ↑ N Chanishvili, T Chanishvili, M. Tediashvili, P.A. Barrow (2001). "Phages and their application against drug-resistant bacteria". J. Chem. Technol. Biotechnol.) 76: 689–699. doi:10.1002/jctb.438. http://cat.inist.fr/?aModele=afficheN&cpsidt=1096871.
- ↑ D. Jikia, N. Chkhaidze, E. Imedashvili, I. Mgaloblishvili, G. Tsitlanadze (2005). "The use of a novel biodegradable preparation capable of the sustained release of bacteriophages and ciprofloxacin, in the complex treatment of multidrug-resistant Staphylococcus aureus-infected local radiation injuries caused by exposure to Sr90". Clinical & Experimental Dermatology 30 (1): 23. doi:10.1111/j.1365-2230.2004.01600.x. PMID 15663496. http://www.blackwell-synergy.com/doi/abs/10.1111/j.1365-2230.2004.01600.x?journalCode=ced.
- ↑ Weber-Dabrowska B, Mulczyk M, Górski A (June 2003). "Bacteriophages as an efficient therapy for antibiotic-resistant septicemia in man". Transplant. Proc. 35 (4): 1385–6. doi:10.1016/S0041-1345(03)00525-6. PMID 12826166. http://linkinghub.elsevier.com/retrieve/pii/S0041134503005256.
- ↑ Mathur MD, Vidhani S, Mehndiratta PL. (2003). "Bacteriophage therapy: an alternative to conventional antibiotics". J Assoc Physicians India 51 (8): 593–6. doi:10.1258/095646202760159701. PMID 12194741.
- ↑ Mc Grath S and van Sinderen D (editors). (2007). Bacteriophage: Genetics and Molecular Biology (1st ed.). Caister Academic Press. ISBN 978-1-904455-14-1 . http://www.horizonpress.com/phage.
- ↑ "Bad Bugs, No Drugs Executive Summary". Infectious Diseases Society of America. http://www.idsociety.org/PrintFriendly.aspx?id=5558. Retrieved 2007-12-11.
- ↑ Wallace RJ (2004). "Antimicrobial properties of plant secondary metabolites". Proc Nutr Soc 63 (4): 621–9. doi:10.1079/PNS2004393. PMID 15831135.
- ↑ Thuille N, Fille M, Nagl M (2003). "Bactericidal activity of herbal extracts". Int J Hyg Environ Health 206 (3): 217–21. doi:10.1078/1438-4639-00217. PMID 12872531.
- ↑ Singh G, Kapoor IP, Pandey SK, Singh UK, Singh RK (2002). "Studies on essential oils: part 10; antibacterial activity of volatile oils of some spices". Phytother Res 16 (7): 680–2. doi:10.1002/ptr.951. PMID 12410554.
- ↑ Stermitz FR, Lorenz P, Tawara JN, Zenewicz LA, Lewis K (2000). "Synergy in a medicinal plant: antimicrobial action of berberine potentiated by 5'-methoxyhydnocarpin, a multidrug pump inhibitor". Proc. Natl. Acad. Sci. U.S.A. 97 (4): 1433–7. doi:10.1073/pnas.030540597. PMID 10677479. PMC 26451. http://www.pnas.org/cgi/content/full/97/4/1433.
- ↑ Shand RF; Leyva KJ (2008). "Archaeal Antimicrobials: An Undiscovered Country". Archaea: New Models for Prokaryotic Biology. Caister Academic Press. ISBN 978-1-904455-27-1. http://www.horizonpress.com/arch.
- ↑ Mukhopadhyay J, Das K, Ismail S, Koppstein D, Jang M, Hudson B, Sarafianos S, Tuske S, Patel J, Jansen R, Irschik H, Arnold E, Ebright RH. (2008-10-17). "The RNA polymerase “switch region” is a target for inhibitors.". Cell 135 (2): 295–307. doi:10.1016/j.cell.2008.09.033. PMID 18957204.
- ↑ Ponte-Sucre, A (editor) (2009). ABC Transporters in Microorganisms. Caister Academic Press. ISBN 978-1-904455-49-3.
External links
- WHO fact sheet
- CDC Article on Hospital Acquired MRSA
- CDC Article on Community Acquired MRSA
- CDC Guideline "Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006"
- ReAct Action on Antibiotic Resistance
- Vancomycin Resistant Enterococcus—Guidelines for Healthcare Workers
- Alliance for the Prudent Use of Antibiotics
- Cox LA, Popken DA (February 2006). "Quantifying potential human health impacts of animal antibiotic use: enrofloxacin and macrolides in chickens". Risk Anal. 26 (1): 135–46. doi:10.1111/j.1539-6924.2006.00723.x. PMID 16492187.
- Prudent Use of Antibiotics
- Information about phage therapy – a possible alternative to antibiotics in case of resistant infections
- Antibiotic-resistance genes as markers Once necessary, now undesirable
- CBS Article on Phage Therapy and Antibiotic Resistance
- Hospitals: Breeding the Superbug? Article on MRSA infections in hospitals, Allianz Knowledge, May 2008
- BURDEN of Resistance and Disease in European Nations - An EU-Project to estimate the financial burden of antibiotic resistance in European Hospitals
- Extending the Cure: Policy Research to Extend Antibiotic Effectiveness
- 2003 New Guidance for Industry on Antimicrobial Drugs for Food Animals Questions and Answers, U.S. FDA
- SciDev.net Antibiotic Resistance spotlight The Science and Development Network is an online science and development network focused on news and information important to the developing world
- Do Bugs Need Drugs?
- Uppsala university, Resistance to antibiotics – global threat
|
|||||||||||||||||